Defending the Front Line
Defending the Front Line
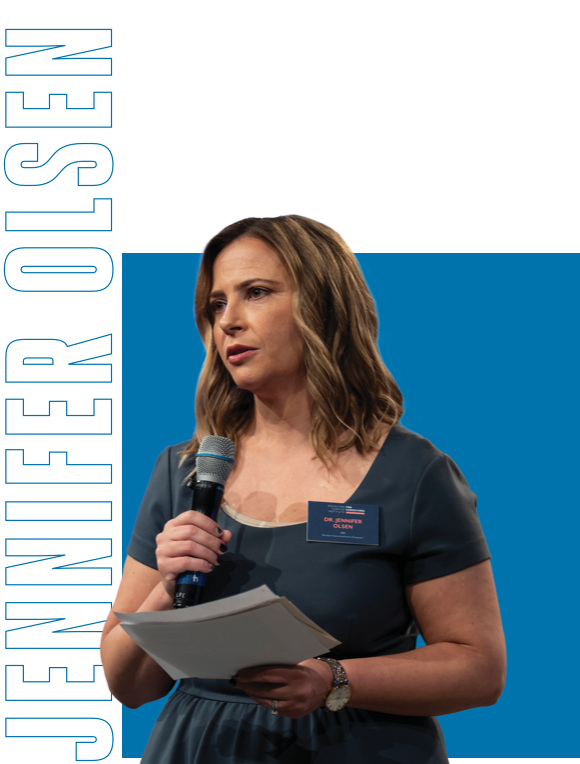
Through her work with the Rosalynn Carter Institute, Jennifer Olsen, M.P.H. ’04, is combating a new kind of public health crisis: underserved caregivers.
by Caite Hamilton
More than a decade into her career as an epidemiologist, Jennifer Olsen decided to take a step back. Her grandmother had been diagnosed with Alzheimer’s disease and her mother had chosen to oversee her care.
“I wasn’t the primary caregiver for my grandmother, but I was trying to find ways to help my mom,” Olsen said. “I was caring for the caregiver.”
What she found was a disconcerting dearth of resources for caregivers. Despite there being more than 50 million family caregivers nationwide, Olsen saw that there was surprisingly little support for this shadow workforce.
Until, that is, she came across the Rosalynn Carter Institute for Caregivers, a nonprofit organization that “promotes the health, strength and resilience” of America’s caregivers. Today, she serves as its CEO.
Rosalynn Carter established her eponymous institute for caregivers in 1987. The former first lady had spent much of her husband’s Georgia governorship and presidency advocating for mental health reform, helping to bring about the Mental Health Systems Act of 1980 through her work on the President’s Commission on Mental Health and, later, working to pass legislation that requires equal coverage of mental and physical illnesses when insurance policies include both. By the end of the 1980s, with many of the programs she’d implemented well underway, she turned her attention to caregiving.
Carter is often famously quoted saying, “There are only four kinds of people in the world: those who have been caregivers, those who are currently caregivers, those who will be caregivers and those who will need caregivers.” She understood a fundamental truth that, even now, often escapes the public consciousness: that caregivers—a friend, family member or neighbor caring for someone who is ill, aging or disabled—are the invisible front line of the national health care system.
“Without [caregivers], where would our country be?” Carter asked in testimony before the Senate Special Committee on Aging in 2011. “The demand for institutional care would increase dramatically and so would the overall costs. Our already over-taxed health care system would be hard pressed to find the workforce necessary to deliver high-quality institutionalized care. And millions more older people would have to live out their final days deprived of the comfort and security of being in their own homes.”
Carter noted that not only do up to 50 percent of caregivers report struggling with depression (and the rates are even higher when caring for someone with dementia), but caregivers report chronic conditions—such as heart disease, cancer and diabetes—at twice the rate of their non-caregiving peers. This is, in part, because the job of a caregiver can be vast and all-consuming, including fulfilling day-to-day tasks as well as overseeing significant clinical health needs.
“Caregiving itself can mean everything from going and getting the mail and shoveling the snow to really complicated medical tasks like infusion treatments and IV changes in the household,” Olsen said. “It’s pretty broad in terms of the types of things that you could do in that role, with both medical task elements and financial and insurance challenges.”
Carter knew the effects of caregiving firsthand, having witnessed her father’s death from leukemia when she was just 13. In her Senate testimony, she recalled running to the outdoor privy to cry, burdened by the task of caring for her father at such a young age. Less than a year later, her grandmother died, and her grandfather came to live with their family. Carter’s mother became his caregiver until he passed away at age 95. The last few years of his life, Carter said, her grandfather was totally dependent on caregiver support.
Much in the way the former first lady launched RCI out of her direct experience with caretaking and the challenges therein, Olsen came to RCI following her own time in the caretaking space. She had spent her career gaining the skills it would take to converge on this long-neglected public health issue.
As CEO of the Rosalynn Carter Institute for Caregivers, Jennifer Olsen pushes for a public health approach to support the nation’s 50 million caregivers.
Olsen’s interest in public health dates back to high school, when she contracted chicken pox on her first day. The experience piqued her interest.
“Why didn’t I get chickenpox when everybody else did? Why is this happening now?” she remembers asking herself. “I’ve always been interested in the intersection of who gets sick, when they get sick and how they get sick.”
That curiosity led her to a degree in biomathematics from Rutgers University and a master’s in public health from GW.
After stints at the Department of Defense and U.S. Department of Health and Human Services, she earned her DrPH from the University of North Carolina at Chapel Hill. She then took a job with Skoll Global Threats Fund. Established by eBay founder Jeff Skoll, the foundation collaborated with academic and community partners to find new ways to detect outbreaks faster. Olsen worked mainly in the area of pandemics, focusing on the animal populations (where outbreaks often originate) in Southeast Asia and East Africa.
One of her proudest achievements in that role was recognizing the need for farmers and mechanics to work together to identify and report early outbreaks.
“Why mechanics? Because people spend a lot of time sitting in those shops waiting for their motorcycle to be ready, so a lot of news flows through those places,” Olsen said. “That job taught me that you can have amazing technology funded by Silicon Valley, but it still requires engagement with the local community to find outbreaks faster.” It was around that time that Olsen began trying to find more ways to support her own family, who had begun caring for her grandmother with Alzheimer’s disease and her uncle with multiple chronic health conditions.
In 2017, she stepped away from her position to be another set of hands for her loved ones.
“I realized that there aren’t very many resources for friends and family who are caring for someone, despite all that health training, all that public health knowledge,” Olsen said. “It seemed like there was nothing out there.” Meanwhile, she was seeing the physical and mental health of her own immediate family members decline.
Her search led her to RCI, which by that time had been advocating in support of this shadow workforce for 30 years. “I saw a job posting and thought, ‘I think I could contribute to solving some of these issues,’” she said.
Olsen traveled to Georgia for the interview, the second half of which was at the home of the Carters.
“I opened the door and [Rosalynn Carter] is standing there with my resume with highlights and notes on it, and I’m just overwhelmed,” she said. Olsen sat down with her and began to explain the ways she felt she could contribute to the institute when President Carter came in. “They both asked me in their own polite ways, didn't I think I'd be a better fit at the Carter Center?”
She understood what they were asking. With her degree in epidemiology, wouldn’t she be more suited for a position at their Atlanta-based organization, where they work in global health and neglected tropical diseases, areas that are more closely related to the work she’d been focusing on her entire career?
“‘I can see why that makes sense,’” she told them. “However, caregivers are a vulnerable population who are at risk for so many health challenges—at greater rates than their non-caregiver peers. So it was very much, at its core, a public health issue.”
She made the case that a public health approach is needed to support the nation’s caregivers and was hired in 2018 as the organization’s executive director. In 2021, she was named its CEO. In her role, Olsen serves as the nonprofit’s brain trust, the driving force behind its initiatives and long-term projects.
“She is truly the visionary behind the work at RCI,” said Megan Shepherd-Banigan, an assistant professor in population health sciences at Duke University and a frequent collaborator with RCI and Olsen. “She can kind of see things 10 steps ahead. She’ll explain an idea she has to me, and it often takes me a couple months to wrap my head around how to actually make it happen. As a trained epidemiologist, she knows it can happen, but it’s so visionary and so out of the box.”
One of those ideas, Shepherd-Banigan said, was to totally reconceptualize the way we think about caregivers. Rather than seeing them as an extension of the care recipient, the project took a caregiver-centered approach, asking: What are the experiences of caregiving? What is the experience like from a caregiver’s perspective?
“The way that caregivers are connected to resources are often in the guise of very siloed medical or social service systems that are very based on the care recipient’s condition,” Shepherd-Banigan said. “We wanted to think about the experiences of caregiving and what it is like from their perspective in a way that is agnostic to the care recipient’s condition.”
“I realized that there aren't very many resources for friends and family who are caring for someone, despite all that health training, all that public health knowledge. It seemed like there was nothing out there.”
With the help of Shepherd-Banigan’s colleagues at Duke, Olsen assembled a team that comprised a physician, a behavioral scientist, qualitative researchers and a health economist. Together, over two years, this kind of fusion cell developed a list of 10 caregiver “profiles,” so instead of being classified as a “dementia caregiver” (which centers on the care recipient), one might be categorized as “managing the decline of an illness” (which centers on the caregiver).
It’s this reimagining of the way we talk about caregivers—and the plight of caregivers—that’s at the core of RCI’s mission.
The three pillars of the organization—support, which provides education in the form of virtual or classroom-style training as well as coaching programs; advocacy, which looks for ways to engage lawmakers at the federal level to think about ways to support caregivers, as with RCI’s current goal of creating a federal Office of Caregiver Health; and initiatives, which entails working with employers and other partners to make sure caregivers are seen and supported in the workplace—are all in service of RCI’s ultimate goal: to create an environment where, as Olsen puts it, “caregivers are able to spend more time holding the hand of the person they’re caring for and less time holding the phone dealing with insurance or doctor’s appointments.”
Like any formidable societal issue, supporting caregivers will require systemic change. Olsen knows the key to caring for caregivers—and easing their burden—is to meet them where they are.
“It’s not that we’re going to make caregiving easy,” Olsen said, “but we want to make it less hard. Part of that speaks to the broad public health principle of engaging with people early and from the preventive space, instead of what we do now, which is wait for caregivers to hit a crisis point. That’s the culture we’re trying to see. That’s the shift we’re trying to make happen.”
Photography: Nicole Craine